Every picture tells a story. Yet it doesn’t tell the full story — especially when a chronic disease like Type 1 diabetes is lurking below the scene. Over the next few months, I’d like to tell some summer mini-stories dedicated to my Aunt Mary Jane, who recently celebrated her 80th birthday with a party in Nellysford, VA.
If anyone lives to the age of 80, they’ve overcome a lot of odds. If you add a Type 1 diabetes diagnosis at age 7, a complete lack of any blood glucose testing systems, and throw in four children to raise, and you’ve got a lifetime challenge. Mary Jane tells me diabetes took over her life one day when her sister, my mother – Cecilia, and her younger brother– John, came home from preschool with the mumps.

My Aunt Mary Jane Dull Hoffman, center, is celebrating her 80th Birthday in April at her homeplace in Nellysford, VA with two of her “favorite” nephews, Phil and me ( Front Right). We are joined by my wife, Lisa, my children Cecilia and Nathaniel, and Phil’s daughter Sammie.
“I’d rather they brought me the mumps, instead,” said Mary Jane. “They got over the mumps in a few weeks. That virus is what cause me to have diabetes for a lifetime. That’s my biggest gripe with diabetes: it’s too much to do. Do this, do that…Every day it’s something else to do. I’ve done a lot of it by the seat of my pants.”
And then Mary Jane smiles: “Since I don’t have my feet anymore, it’s a good thing I’m flying by the seat of my pants most of the time.” After you stop laughing at the irony of a T1D who is a Joslin Medalist honored for “surviving ” diabetes, you see clearly what diabetic complications really mean. Feet are gone. And she’s the lucky one. And then you realize: Diabetes continues to suck and if I don’t manage my Type 1 like a mad man — I could lose my feet and a lot more.
Here’s my goal in highlighting Mary Jane’s story: To show that surviving Type 1 diabetes requires effort, luck and stubborn commitment to each day being better than the day before. In order to beat diabetes — which we have not done yet — a person also needs a healthy dose of kiss-my-butt craziness. When you’re sick on the inside but you look perfectly “healthy” on the outside, it’s not easy to generate a sense of urgency for more research, more awareness, and more money.
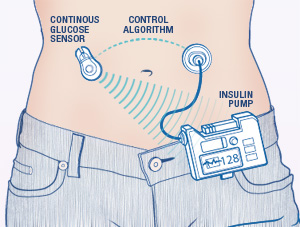
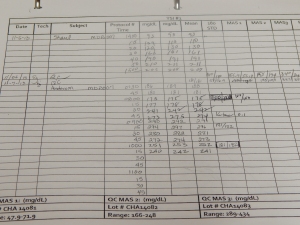
My other goal here: To announce that I’m riding again in the JDRF RIDE FOR A CURE at Amelia Island, FLA on Oct. 30, 2016 and that all the money I raise — thanks to all my compassionate supporters — will go to JDRF and its support of Dr. Boris Kovatchev and the researchers at the Center for Diabetes Technology at the University of Virginia. The CDT team in Charlottesville is part of a five member university consortium still trying to bring an Artificial Pancreas System to reality. Funds raised support worldwide human clinical trials required to convince the FDA that it’s time to approve an AP or a bionic pancreas which will deliver better glucose control and fewer serious medical complications to persons living with T1D.
(I will add a blog update on my current participation in the ” Project Nightlight” Home AP trial — 3 weeks are done and the closed loop is working exactly as advertised — nighttime under control.)
I’m not a young man any more — so it comes down to this: My marathon journey for a cure has become a sprint to the finish line. It’s like the riding the final stage. Aunt Mary Jane was promised a cure when she was first diagnosed in the 1940s. Seventy years later, the promises are still being made and we’re still pedaling up hill with our real and artificial feet!
Aunt Mary Jane and I may not cross the ultimate finish line — A cure to Type 1 diabetes without tech solutions, but we want to be counted as two people who tried to make it happen. Together, We R the Cure.