The VC-01 combination product is expected to be implanted under the skin of the patient through a simple outpatient surgical procedure. The cells are then expected to further differentiate to produce mature pancreatic cells that will synthesize and secrete insulin and other factors, thereby regulating blood glucose, commonly referred to as blood sugar levels.
In the closing paragraph of my last blog post, I tried to strike a balance between hope and realism when describing ViaCyte’s VC-01 combination product and pending clinical trials aimed at a virtual cure for Type 1 diabetes.
The possibility/probability of successful clinical trials makes you anxious, optimistic, and fearful of another big letdown. It also leaves you with lots of questions. So I contacted ViaCyte to say “Thank You” for presenting at the JDRF Research Summit in Bethesda, MD last month and asked a few follow-ups. To my delight, I got an email response from a person named “Howard” at the San Diego-based company.
Q: How will you recruit or identify prospects for the upcoming clinical trials?
A: Currently, ViaCyte is still in preclinical development with our diabetes product VC-01; we are not conducting any clinical trials at present. However, we do anticipate completing the necessary preclinical studies and filing an application with the FDA so as to be able to proceed with human trials sometime later this year. Note that when the clinical trial starts, ViaCyte will adhere to Good Clinical Practice (GCP) guidelines, which preclude the Sponsor (ViaCyte) from having direct contact between clinical study subjects.
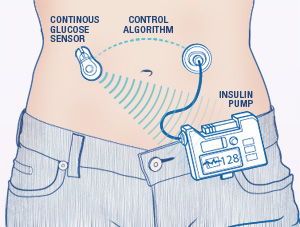
Q: How does the proprietary device ” KNOW” when and how much insulin to release? Are the stem cells smart enough to automatically ” sense ” the amount of glucose in the body and respond in a measured fashion just like a healthy pancreas does in non Type 1 Diabetics?
A: Yes, the cells contained in the device are smart enough to know when to secret insulin. Strictly speaking, the cells in the device are not stem cells. They are derived from stem cells but have undergone differentiation to a point where they are no longer considered stem cells. The most current information about our progress and technology can be found on our website.
Q: Will clinical trial participants be required to take immunosuppressant drugs, and, if this therapy works, will these drugs be required for the rest of the patient’s life?
A: At the present time we do not anticipate that any immunosuppressive therapy will be required, either during the clinical trial or at any time thereafter.
Q: Is there an age range for eligible human trial participants? If people are interested in the clinical trial or applying, how do they contact ViaCyte?
A: In our first clinical trial we anticipate that the age inclusion range will be from 18 – 55 years. Once clinical trials start, information on the location of clinical study sites will be available online at clinicaltrials.gov, the US government database of current clinical trials. Additionally, information should be available on our website once the trial is closer to launch.
Q: Finally, how will this implantable device actually cure my diabetes?
A: By acting essentially as a replacement endocrine pancreas, the source of insulin and other regulatory hormones produced in our bodies, ViaCyte’s VC-01 combination product has the potential to be a virtual cure for type 1 diabetes. The VC-01 therapy is the combination of:
- PEC-01 cells: A proprietary pancreatic endoderm cell product derived through directed differentiation of an inexhaustible human embryonic stem cell line, and
- Encaptra drug delivery system: A proprietary immune-protecting and retrievable encapsulation medical device.